ITB Syndrome – How to resolve runners’ knee
So, after all the mental and physical preparation for your weekend run, you go out planning to do a 10k jog. Halfway through, you feel a sharp pain on the outside of your knee and you suddenly have to stop. Thoughts like ‘’Just my luck’’ and ‘’I should have just stayed in’’ enter your head as you hobble back home. You may wonder if you’ve knocked it (but haven’t) or if you’ve been kneeling too much, which only adds to the confusion, but there is another possibility.
As an osteopath, I see a lot of patients with knee issues, and because of the demographics of runners and cyclists that simply want to get fit, I see a lot of frustrated individuals. This is primarily because it is so painful and it greatly affects running, which for a lot of people is a go-to stress reduction activity, but also because it’s an unknown entity. A lot of patients I see have Google’d the issue and believe they may have damaged their cartilage or ligaments, which sounds very serious when you read certain articles. I am here to tell you that it could simply be ITB syndrome, otherwise known as ‘’runners’ knee’’.
ITB (iliotibial band) syndrome is rife amongst recreational and elite runners and cyclists. It is a source of frustration in 52% of runners, and is responsible for 16% of all running injuries. It’s also the 3rd most common injury that runners and cyclists suffer (1).
So what is it?
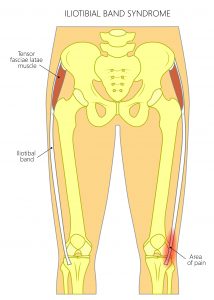
The ITB is a band of fibrous tissue that connects the hip muscles to the lower leg. When the mechanics of the hip aren’t balanced properly, which is a very common phenomenon. This is especially true in runners and cyclists, the ITB thickens and rubs against the outside of the knee. This is where there is a fat pad. This fat pad is highly pain- sensitive and prone to inflammation, which is what causes the pain.
Why is it occurring?
The excessive friction can occur for a few reasons:
- Rapid change in mileage
- Hill sprinting
- Running on a tilted surface
- Glute weakness
- Foot pronation
- Allowing the knee to bend inwards
- Bow legs (2)
How do you know if you actually have it?
Usually a patient with ITB syndrome comes to the Clinic with no previous history of trauma. This includes knocks or twists to the knee, but they may have recently increased their running activity. The pain can typically occur a few miles into the run and the pain worsens as they continue, especially at heel strike at around 30 degrees of knee flexion (3). If this sounds like you, please get in contact with an appropriate medical professional.
As 80% of the diagnosis comes from who the patient is and what they say, ITB syndrome is no different. Furthermore, clinical testing for ITB syndrome is weak and unreliable with only one or two tests that have been subjected to scientific testing.
Regarding the next step if it doesn’t get resolved, scans can help diagnose the inflammation on the fat pad. Most patients won’t require this as the clinical presentation and area of pain is usually enough to confirm ITB syndrome.
How to resolve it
The obvious treatment would seem to be to reduce the inflammation, so rest and ice and maybe medication. Despite this logical argument, that doesn’t seem to be the most reliable way of resolving the problem. The best interventions usually get to the true source of the issue. This is because the poor hip mechanics contribute to the tightness in the ITB and therefore the compression on the fat pad, good hip strength and conditioning works the best.
Osteopaths, physiotherapists and sports therapists will have to assess which muscles aren’t working before a rehab plan is put in place. However, at the Movement and Wellbeing Clinic we put a full management plan in place so that you will feel confident about the situation and you are empowered to help yourself to resolve it. Usually the program of exercises will be gluteus medius strengthening and specific knee stability work, but again this depends on the assessment.
In terms of hands-on treatment, it is common to see the problematic knee over-rotate inwards which requires hands-on specific mobilisation. This can be a great tool to combat ITB syndrome and keep it at bay, alongside the exercises.
Lifestyle advice
Modifying activity is a big part of resolving ITB syndrome: we have two options depending on the case:
- Modify running distance
- Modifying running technique
- Complete rest for a period of time
The three options will be discussed with you and the decision will be made together. Like our philosophy with most musculoskeletal conditions, treatment must make sense to you. For example, we’re not going to tell you to stop running completely if the pain isn’t severe and you have a race planned. Conversely, we’re not going to ask you to carry on through the pain if you’re just doing recreational exercise and there is no obvious benefit in continuing with running in the short term.
For any further questions, please don’t hesitate to ask:
0161 209 2980
info@movementandwellbeingclinic.co.uk
Ed Madeley M.Ost
References
- Noehren B, Davis I, Hamill J. ASB clinical biomechanics award winner 2006 prospective study of the biomechanical factors associated with iliotibial band syndrome. Clin Biomech (Bristol, Avon). 2007 Nov;22(9):951-6.
- Fredericson M, Weir A. Practical management of iliotibial band friction syndrome in runners. Clin J Sport Med. 2006 May;16(3):261-8
- Ferber R, Noehren B, Hamill J, Davis IS. Competitive female runners with a history of iliotibial band syndrome demonstrate atypical hip and knee kinematics. J Orthop Sports Phys Ther. 2010 Feb;40(2):52-8
