Hoffa’s Fat Pad Impingement (Knee Pain)
Knee pain is a highly irritating issue, mainly due to the lack of functional movement you are able to perform with knee pain (walking, going up and down stairs etc.). When you add the burning and insufferable pain from Hoffa’s fat pad you become a very frustrated person requiring help.
The preliminary recognition of the fat pad was first made in 1904 by Dr. Albert Hoffa, who was a German surgeon specialising in lower limb conditions.
Since Dr Hoffa’s recognition, not much research has gone into it, and we still don’t know what it does, or how common, or uncommon, it is. Our understanding of the fat pad improved after research done by Scott Dye et al found that the fat pad is the most pain-sensitive area in the knee. He went into the knees of his test subjects and prodded all the structures inside and got them to score how painful it was. Hoffa’s fat pad was the most painful structure in every participant. Although it was a very useful study, I’m glad I wasn’t subjected to that experiment!
So, why does it happen?
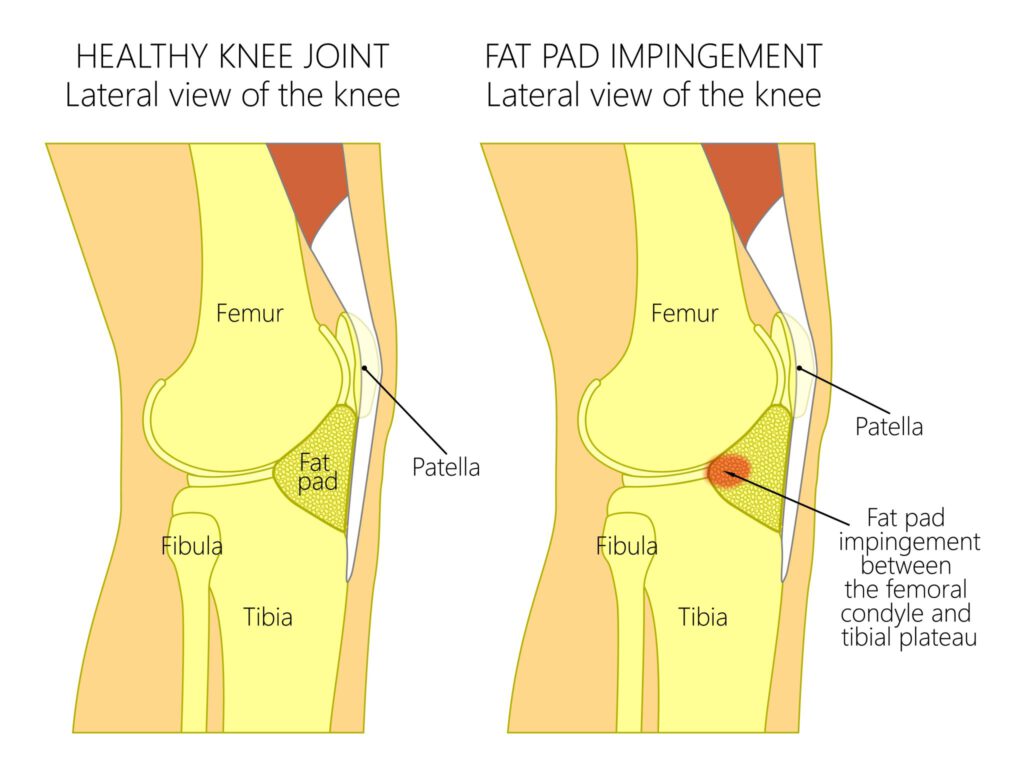
The fat pad is spongy fat tissue located just below the kneecap, which means any bad positioning of the kneecap can compress and irritate it, causing pain.
There are several issues that may result in Hoffa’s fat pad impingement:
- Imbalance in the knee muscles
- Previous kneecap dislocation
- Previous trauma of the kneecap
- Hypermobility
How do I know if my pain is coming from the fat pad?
Typically, patients with Hoffa’s fat pad pain complain of highly-irritating pain. Even with the slightest of movement or pressure over the right (or wrong) area. If you are an extreme amount of discomfort, Hoffa’s fat pad impingement should be considered. The movements in particular that irritate are standing, walking barefoot or in a heel, and the final part of straightening the leg. Another major symptom is swelling around the knee, which is due to the inflammation around the fat pad.
Looking into how the incident occurred is important, and with Hoffa’s fat pad pain, the patient has usually had a direct blow to the knee, a forced banding backward of the knee, or previous knee surgery (especially knee arthroscopy). If you haven’t experienced an impact injury or surgery, when you visit the clinic, your osteopath or physiotherapist will decide if you fit one of the following associated categories:
- Patella (kneecap) instability – causes the kneecap to ‘bash’ into the fat pad, because it is unstable
- Lateral fat pad pain – causing the kneecap to pinch on the fat pad because it is held in an undesirable way.
How do we resolve it?
First of all, establishing an accurate diagnosis is highly important. This is because if the pain is coming from the tendon (tendinopathy), we encourage the pain to increase as we treat it. With Hoffa’s fat pad you’ll be making it worse by increasing the pain. Once we’ve diagnosed that it is a Hoffa’s fat pad, there will be a full explanation of what it is. The prognosis is also important, because there is an anxiety in fat pad patients. This may be due to the level of pain that is present.
After explaining the management plan, as always patient compliance in fulfilling their obligations is huge. Especially with fat pad pain, as 95% of the treatment of it comes from outside the clinic room.
If you’ve experienced a direct trauma, the most important thing to do is take the load off. This includes choosing appropriate footwear and reducing all movements that would result in pain. Regarding footwear, usually patients struggle in flat heels, socks or barefoot, so using footwear with a heel should help. Ice massage also is very beneficial and can reduce the inflammation. You can do this before the visit to your osteopath or physiotherapist.
Kneecap instability group patients (where there hasn’t been a trauma) require all unnecessary movement in the leg, while strengthening the quads in a dynamic way. Lateral fat pad pain patients have a tightness in the structures on the outside of the knee, which would need ‘’loosening’’ through manual therapy.
Finally, there is a correlation between being overweight and fat pad pain, so taking steps to mitigate this is advisable. If you require help with weight loss, we may be of assistance.
Should I get a scan or surgery?
So, the clinical evidence suggests MRI imaging results don’t necessarily paint the full picture. And unless you match with the typical presentation of having a Hoffa’s fat pad, a scan should be put on hold. This is mainly due to image results showing inflammation of the fat pad, but no pain or reduction in function.
Surgery is advised if treatment mentioned above is not working.
For any further questions, please don’t hesitate to ask:
0161 209 2980
info@movementandwellbeingclinic.co.uk
Ed Madeley M.Ost