Sciatica and How to Treat it
Sciatica and how to treat it
One of the more commonly repeated ‘Google diagnoses” is sciatica. But what does it actually mean?
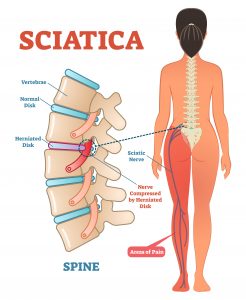
Sciatica is a debilitating condition in which the patient experiences pain and/or paresthesias in the distribution of the sciatic nerve or an associated lumbosacral nerve root
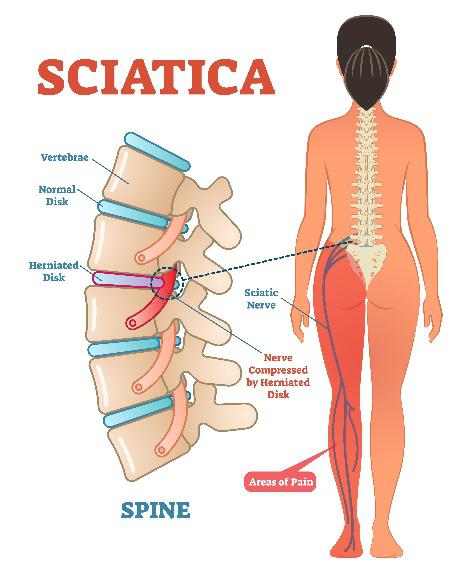
First of all, the term sciatica isn’t a diagnosis, it’s a symptom which can lead to a true diagnosis. Having sciatica doesn’t really paint the big picture as there could be various reasons for the symptom. The definition above is quite specific, and it certainly doesn’t account for all types of back pain. A lot of the confusion around of the term is due to what the patient is feeling. This can also appear in a lot of different types of back pain. What needs to be assessed is the tissue compressing the sciatic nerve, this diagnosis doesn’t always mean the dreaded slipped disk.
You are just as likely to develop sciatica as a man or woman. It has with an annual incidence of 1-5%. It also occurs more frequently in truck drivers and machinery operators (mainly jobs that requires a person to adopt an awkward position), particularly if you are in your 40s.
In clinic, patients presenting with sciatica typically come in complaining of a deep, burning pain in the buttock, alongside an altered sensation (and sometimes a heaviness) in the same side of the leg with occasional weakness. I’m commonly asked what exercises the patient should be doing to prevent sciatica. The answer to this is, if you have no prior symptoms, strenuous physical activity. However, if you have symptoms then physical activity can make it worse – be careful and always seek professional help before carrying out any treatments.
The sciatic nerve
The sciatic nerve is the longest and largest nerve in the body and can get up to three quarters of an inch thick. It is responsible for bringing your heel up your buttock, as well as contributing to the sensation in your foot and lower leg. The sciatic nerve is a bit like the M6, as you can see in the picture to the right, it is a thick band as it branches off to contribute to a lot of areas of the leg.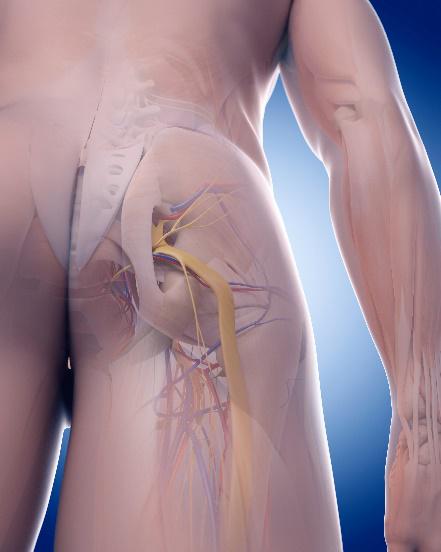
Along the route to the leg, 22% of people’s sciatic nerve pierces a muscle called the piriformis. This is significant in piriformis syndrome, which can cause sciatica when the muscle gets tight.
What could be causing my sciatica?
Unfortunately, if you’re experiencing the symptoms the most likely outcome is that it’s a slipped disc. The sciatic nerve pierces the piriformis muscle in 22% of patients, which would result in compression of the nerve. If this is you, you’re lucky as this should be a lot easier to resolve!
Lumbar spinal stenosis in the elderly population can contribute to sciatica. Spinal stenosis is a condition where the disc shrinks and compresses the nerve where it comes out of the spine.
Spondylilothesis, which is a slippage of the actual vertebrae (not the disc, the actual bone) can contribute as it forms a misalignment of the vertebra, therefore impinging on the hold (foreman) in which the sciatic nerve exists.
So, how do we get you better?
First of all, a big principle we have at the clinic is explanation. A good solid explanation with education is vital for the therapist/patient partnership. General advice initially is to avoid strenuous activity and periods of prolonged sitting/standing. Movement seems to be key according to the research.
Manual treatment alongside an exercise program is the most beneficial option, the osteopath will address the muscle tightness, while incorporating pelvic balancing techniques to facilitate stability. Alongside this, the exercise program will address the deficiencies found in the assessment. Core stability and switching on of pelvic stability muscles are common exercises.
Typically, patients should expect to see improvements in 6-12 weeks. No improvement in 6 weeks should result in referral for scan to assess the damage.
Any questions, please email Ed on:
info@movementandwellbeingclinic.co.uk